Initiated in 2018 with support from the National Institute of Aging, Sleep Profiler now has the capability to longitudinally assess brain health by profiling specific neurodegenerative disorders. These ongoing research efforts were conducted in collaboration with an international research consortium. The capabilities were designed to satisfy the >85% of older adults who want to know if they are at-risk for a neurodegenerative disorder so they can plan for their future.
Our scientific discoveries are highlighted in multiple peer-reviewed manuscripts which include the description of a new sleep biomarker called non-REM hypertonia (NRH), findings demonstrating a relationship between NRH and REM sleep without atonia, and studies which investigate the relationship between NRH vs. sleep spindle activity and autonomic dysregulation.

We cross-validated the automated staging accuracy in patients with isolated REM sleep behavior disorder and investigated whether a biomarker developed to detect ICU delirium, called atypical N3 sleep, was able to assess altered mental status in patients with Lewy body dementia. The association between sleep and wake EEG slowing attributed to neurodegeneration was also described.
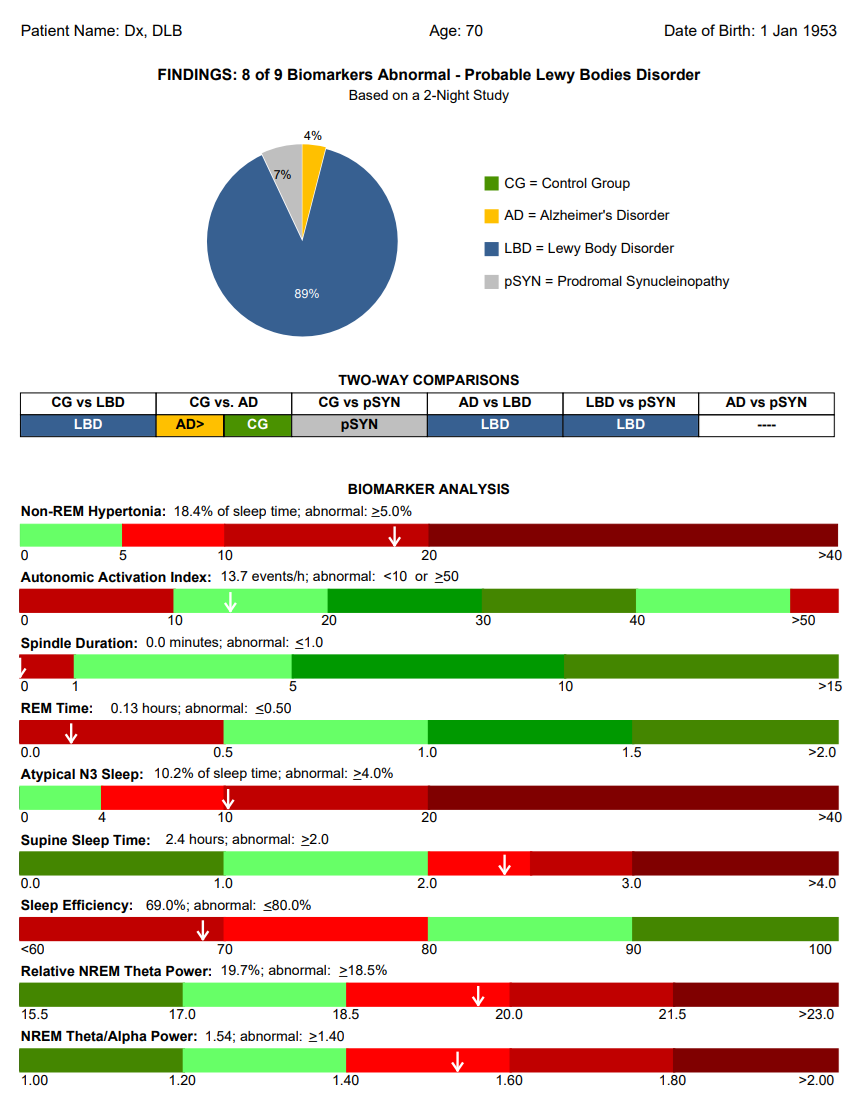
Additionally, the association between supine sleep and neurodegenerative disorders, first reported by our consortium in 2019, has now been confirmed in independent cohorts with Lewy body Disease, Alzheimer's disease, and Mild Cognitive Impairment. A proposed mechanism of action, as well as a strong relationship between supine sleep and disease duration and motor impairment in Parkinson’s patients further supports our initial finding.
Finally, a community-based survey identified what physicians should and should not do to assist their patients in matters related to neurodegenerative disorders.
The 20-min video below summarizes the accuracy and reliability of the neurodegenerative disorder risk and severity assessment, and changes that occur in at-risk patients.